
Differentiation of Nijmegen breakage syndrome from Fanconi anemia
V.B. Rao, L. Kerketta, S. Korgaonkar and K. Ghosh Genet. Mol. Res. 6 (3): 622-626 (2007) ABSTRACT. Nijmegen breakage syndrome (NBS) is a rare auto-somal recessive condition with chromosomal instability. Clinical and biological overlap between Fanconi anemia and ataxia telangiectasia has been reported. We report two cases of NBS born to consanguineous parents. Case one had NBS and Falconi anemia clinical features but relatively little chromosome breakage. The second case had mild NBS features, while cytogenetic evaluation with mitomycin C induction showed chromosome damage. Chromosomal analysis of bone marrow cells revealed tetraploidy, which indicates progression towards leukemia. On the basis of clinical and cytogenetic evaluation, these two cases were confirmed as NBS. However, detailed molecular studies are essential for accurate diagnosis and management of this disease. Key words: Chromosomal breakage, Nijmegen breakage syndrome, Fanconi anemia, Tetraploidy INTRODUCTION Nijmegen breakage syndrome (NBS) is a rare autosomal recessive condition with chromosomal instability. The clinical manifestations include microcephaly, dysmorphic features, growth retardation, recurring infections, immunodeficiency, spontaneous chromosome breakage and hypersensitivity to ionizing radiations, and high risk of malignancies. NBS was first recognized in 1981 in two siblings with microcephaly, short stature, skin pigmentation abnormalities, mental retardation, and immunological defects (Weemaes et al., 1981; TINBSSG, 2000; Varon et al., 2000). NBS is a rare disease and is most common in Polish people and in those of Solvic origin. NBS patients have founder mutation 657del5 in the NBS gene (Varon et al., 1998). However, the clinical and biological overlap between Fanconi anemia (FA) and ataxia telangiectasia (AT) has been reported (Gennery et al., 2004; New et al., 2005). CASE 1 An 11-year-old girl was referred for chromosomal analysis because of short stature. The proband was second born to consanguineous parents. The mother’s age was 24 years and the father was 39 years at the time of birth. The mother had a history of three spontaneous abortions. On examination, proband height was 97 cm, weight 14 kg, and head circumference 41 cm. The upper and lower segment measurements were 41 cm and 56 cm, respectively. The bone age was 3.9 years and arm span was 96 cm. The proband had short stature, microcephaly, dysmorphic features, a bird-like face, lack of eyelashes, macules on the chest, and skin infections since childhood. The patient had short limb dwarfism, short fingers and pustule on the dorsum of the right palm. The bone age was 3.9 years. The large patent ductus arteriosus was operated at six months of age. Ultrasound of the abdomen and pelvis revealed a hypoplastic uterus and normal ovaries. Hormonal evaluation of the proband revealed elevated levels of thyroid-stimulating hormone (>5.0) and decreased levels of T4 (0.91 µg/µL). T3 and follicle-stimulating hormone levels were within normal range. Anti-transglutaminase (IgG) was high (192.3 µL). CASE 2 The proband was an 8-year-old girl born to consanguineous parents. The mother’s age was 18 years and the father was 25 years at the time of birth. On examination, proband height was 12 kg, height 110 cm, and head circumference measurement was 46 cm. The proband had short stature, a bird-like face, microcephaly, and hyper-pigmented elevated lesions on the body. The proband also had delayed bone age (three years) and hypoplastic ovaries and uterus. Thyroid hormonal levels were found to be within the normal range. Immunoglobulins (IgG and IgM) levels were low. CYTOGENETICS Cytogenetic studies were performed on peripheral blood lymphocyte cultures stimulated with phytohemagglutinin on peripheral blood cultures induced with mitomycin C (MMC) (40 ng/mL). Blood cultures were made from an FA patient and from age- and sex-matched controls. Chromosomal analysis of the proband revealed spontaneous chromosomal breakage and fusion, most frequent in chromosomes 7, 8, and 14 (Figure 1). There was a slightly elevated frequency of chromosomal breakage in cultures treated with MMC compared to controls; however, the breakage frequency was low when compared to that in the FA patient. Chromosomal analysis of sib and parents revealed normal karyotypes. In the second patient, the mitotic index was low and there was spontaneous chromosomal breakage. The MMC-induced cultures showed a high frequency of chromosomal breakage compared to controls. However, the breakage frequency was low compared with that in the FA patient. The patient was followed up at three-month intervals, and after one year there was no change in chromosome damage frequency. The bone marrow (BM) aspiration showed leukemia development. The immunophenotype revealed T-cell acute lymphoblastic leukemia (ALL). The chromosomal analysis from the BM sample revealed a tetraploid karyotype (Figure 2). 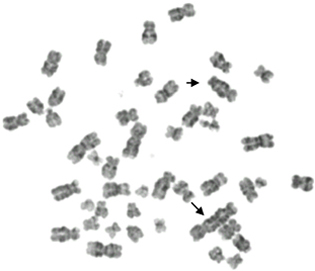
Figure 1. Metaphase of a cell from a patient with Nijmegen breakage syndrome showing spontaneous chromosome breakage and fusion (arrows). 
Figure 2. Metaphase of a cell from a patient with Nijmegen breakage syndrome showing tetraploidy in bone marrow cells. DISCUSSION NBS diagnosis is based on physical anomalies and chromosomal instability. The classical phenotype of NBS is growth retardation (30%), microcephaly (75%), mental retardation, excessive skin pigmentation, a bird-like face with a prominent mid face, a long nose and receding mandible, and immunodeficiency (Couturier, 1998). Though most of the known clinical features were present in proband one, a different diagnosis was considered, because of clinical overlap between FA and NBS (Gennery et al., 2004; New et al., 2005). In our case 1 except for radius axis defects and hematological abnormalities the patient had all FA clinical features. The rare anomaly of patent ductus arteriosus found in our patient has also been seen in some FA patients. As there was little chromosomal breakage induction in the proband compared to the FA patient, we decided to exclude FA because it shows clinical heterogeneity and considerable overlap with the phenotypes of a variety of other genetic diseases. The second case had major clinical features of FA, such as short stature, and microcephaly; however, the diagnosis was considered as AT and NBS on the basis of immunodeficiency. AT was ruled out because AT blood cultures are reported to be sensitive to radiations and some NBS exhibit low-level chromosome breakage with induction by alkylating agents. As the proband blood cultures induced with MMC showed a high frequency of chromosome damage, the case was diagnosed as NBS. Both NBS and AT patients display similar combined immunodeficiency and specific chromosomal rearrangements that frequently involve chromosomes 7 and 14 (van der Burgt et al., 1996). Radiosensitivity is also a common cytogenetic hallmark of AT and NBS homozygotes (Wegner et al., 1999). In our case 1, chromosomes 14 had frequently chromosome breakage. However, AT diagnosis was ruled out due to an absence of neurological abnormalities. Both cases were diagnosed as NBS on the basis of clinical correlation with cytogenetics. Chrzanowska et al. (2001) reported an NBS case with a typical clinical picture with absence of microcephaly and presence of a congenital heart defect and preaxial polydactyly. Recently, monozygotic twin brothers with a severe form of NBS without chromosomal instability have been reported and molecular studies revealed compound heterozygosity for the major 657 del5 mutation in these twins (Seemanova et al., 2006). Malignancy is the most common cause of death in NBS patients. Most malignancies are of lymphoid origin and develop in patients younger than 20 years. Non-Hodgkin’s lymphomas, ALL and Hodgkin’s disease are the most common. However, two cases of acute myeloblastic leukemia were also reported. We have followed up case 2; on the basis of a complete blood count the case was diagnosed as leukemia. The BM biopsy smear was suggestive of ALL. Chromosomal analysis of the BM revealed a tetraploid karyotype; tetraploid is frequently reported in ALL patients. The ploidy and DNA content of leukemic blast cells are well-established prognostic markers of childhood ALL (Moorman et al., 2003; Harrison et al., 2004; Sutcliffe et al., 2005). Higher hyperdiploidy (51-65 chromosomes) is usually associated with low-risk features and is reported to have a good prognosis (Moorman et al., 2003; Harrison et al., 2004). However, according to the literature, tetraploid ALL appears to be associated with a T-cell phenotype and has poorer prognosis compared with other ploidy groups (Pui et al., 1990; Raimondi, 1993). Hence, early detection of leukemia in NBS patients is important for management of the disease. REFERENCES Couturier J (1998). Nijmegen breakage syndrome. Atlas Genet. Cytogenet. Oncol. Haematol. October 1998. URL:http://AtlasGeneticsOncology.org/Kprones/NijmegenID10020.html Chrzanowska KH, Stumm M, Bekiesiska-Figatowska M, Varon R, et al. (2001). Atypical clinical picture of the Nijmegen breakage syndrome associated with developmental abnormalities of the brain. J. Med. Genet. 38: E3. Gennery AR, Slatter MA, Bhattacharya A, Barge D, et al. (2004). The clinical and biological overlap between Nijmegen breakage syndrome and Fanconi anemia. Clin. Immunol. 113: 214-219. Harrison CJ, Moorman AV, Broadfield ZJ, Cheung KL, et al. (2004). Three distinct subgroups of hypodiploidy in acute lymphoblastic leukaemia. Br. J. Haematol. 125: 552-559. Moorman AV, Richards SM, Martineau M, Cheung KL, et al. (2003). Outcome heterogeneity in childhood high-hyperdiploid acute lymphoblastic leukemia. Blood 102: 2756-2762. New HV, Cale CM, Tischkowitz M, Jones A, et al. (2005). Nijmegen breakage syndrome diagnosed as Fanconi anaemia. Pediatr. Blood Cancer 44: 494-499. Pui CH, Carroll AJ, Head D, Raimondi SC, et al. (1990). Near-triploid and near-tetraploid acute lymphoblastic leukemia of childhood. Blood 76: 590-596. Raimondi SC (1993). Current status of cytogenetic research in childhood acute lymphoblastic leukemia. Blood 81: 2237-2251. Seemanova E, Sperling K, Neitzel H, Varon R, et al. (2006). Nijmegen breakage syndrome (NBS) with neurological abnormalities and without chromosomal instability. J. Med. Genet. 43: 218-224. Sutcliffe MJ, Shuster JJ, Sather HN, Camitta BM, et al. (2005). High concordance from independent studies by the Children’s Cancer Group (CCG) and pediatric Oncology Group (POG) associating favorable prognosis with combined trisomies 4, 10, and 17 in children with NCI standard-risk B-precursor acute lymphoblastic leukemia: a Children’s Oncology Group (COG) initiative. Leukemia 19: 734-740. TINBSSG (The International Nijmegen Breakage Syndrome Study Group) (2000). Nijmegen breakage syndrome. Arch. Dis. Child. 82: 400-406. van der Burgt I, Chrzanowska KH, Smeets D and Weemaes C (1996). Nijmegen breakage syndrome. J. Med. Genet. 33: 153-156. Varon R, Vissinga C, Platzer M, Cerosaletti KM, et al. (1998). Nibrin, a novel DNA double-strand break repair protein, is mutated in Nijmegen breakage syndrome. Cell 93: 467-476. Varon R, Seemanova E, Chrzanowska K, Hnateyko O, et al. (2000). Clinical ascertainment of Nijmegen breakage syndrome (NBS) and prevalence of the major mutation, 657del5, in three Slav populations. Eur. J. Hum. Genet. 8: 900-902. Weemaes CM, Hustinx TW, Scheres JM, van Munster PJ, et al. (1981). A new chromosomal instability disorder: the Nijmegen breakage syndrome. Acta Paediatr. Scand. 70: 557-564. Wegner RD, Chrzanowska K, Sperling K and Stumm M (1999). Ataxia-telangiectasia variants (Nijmegen breakage syndrome). In: Primary immunodeficiency disease. A molecular and genetic approach (Ochs HD, Smith CIE and Puck JM, eds.). Oxford University Press, Oxford, 324-334. |
|